Laurie's Blogs.
Nov 2020
Tendinopathy - how to address & more!
I found a great podcast on this topic.
It was a discussion / interview with Dr. Ebonie Rio, a researcher at La Trobe University in Australia. It fits is very nicely with a couple of questions I’ve received recently about tendon management. So, I’ll just summarize the interview. P.S. This Podcast is awesome. Look for Physio Explained by Physio Network to hear more great podcasts like this one.
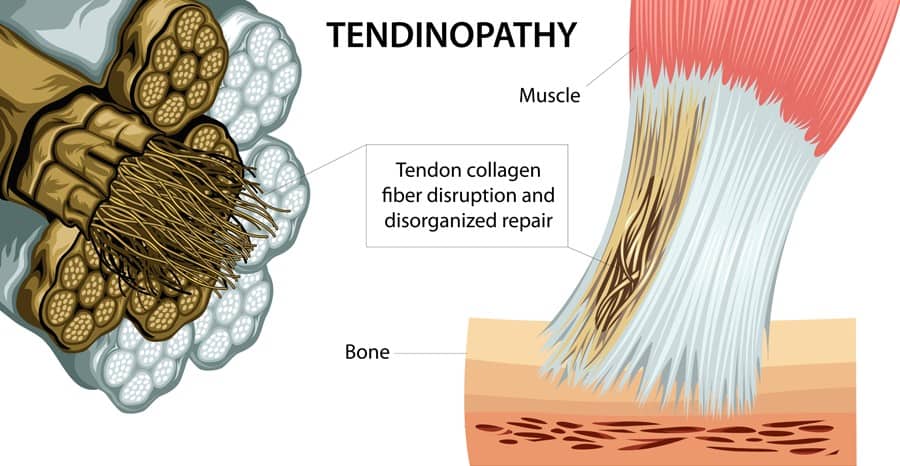
So, Dr. Rio starts out with defining Tendinopathy lesions. They are those that demonstrate pain with high tendon load (i.e. a fast spring type load)… which for the Achilles would be any sort of load based on the biomechanics of how that tendons functions. However, for the patellar tendon would include more of a burst type activity. Tendinopathies have a localized pain (i.e. on palpation or as pointed out by a patient), but with exercise, they ‘warm out’ of the pain. Peritenon pathology however is inflammation of the tendon sheath. It’s different because it is further inflamed with repetitive loading (i.e. the tendon slides within the sheath). So this pathology worsens as exercises continues.
It’s important to differentiate! Tendinopathies need load to heal. Peritenon lesions need reduced movement in order to heal.
Focusing on Tendinopathy: All exercise types have a role, so long as they are patient specific and take into account clinical reasoning. They need to be progressive, and it is smart to combine the different protocols. So, those following the tendinopathy treatment trends will be familiar with the ‘Eccentric is Best’ mantra.
What Dr. Rio is saying (and where research has progressed) is that anything that isometric or slow static loading is okay with tendinopathy. She stated that what is important to take into account is the asymmetry from side to side, not only of the tendons, but of the whole extremity. So that you need to pay attention to making your prescriptions patient specific using clinical reasoning, and to combine the various protocols.
A therapist needs to address the individual deficits, take into account the patient’s previous capacity, goals, and the irritability or pain of the structure. Exercise prescription should be progressive (i.e. increase load as able), and needs to include educations regarding safe load versus provocative load.
One of the old adages from the earlier eccentric protocols research was that pushing into pain was needed. Dr. Rio says that she has adopted a good compromise: Acceptable ‘push’ would result in low and stable symptoms. In other words, we don’t want flare ups as a result of our exercise prescription. The other pearls of wisdom gleaned from this podcast were to think about the brain, spinal cord and the motor cortex and the impact that pain may have had on these structures. As such, retraining and relearning normal use or ‘fear of pain’ behaviours may need to be addressed.
And lastly, stop using the word ‘Tendinitis’. It implies inflammation which leads to entirely inaccurate thoughts and actions in regards to treatment. All in all, this was a great little refresher / update podcast on tendons. I hope this inspires your week ahead!
Cheers! Laurie


