Laurie's Blogs.
Aug 2020
Myopathy & Delayed Tendon Healing in Medically Challenged Patients
The following question was sent to me via e-mail.
Is there any research to support or dispute there is delayed scarring in for dogs that have Cushing’s disease, Diabetes, obesity or even old age with cranial cruciate ligament injuries, dogs with either with an extracapsular surgery or no surgery at all? It seems like more of these pups take longer to create any functional stability from the scar tissue when they have opted for conservative management.
Your thoughts?
So, I did a literature search. The search terms were difficult to decide upon at first, however, I came up with Tendon healing and <> and then Myopathy and <>. Here’s what I found.
Tendon Healing in Patients with Diabetes, Cushing’s, Obesity, or Age
1. Diabetes:
•Diabetes substantially alters bone metabolism and soft tissue healing, posing a risk of adverse fracture healing and other complications.
Gortler H, Rusyn J, Godbout C, Chahal J, Schemitsch EH, Nauth A. Diabetes and Healing Outcomes in Lower Extremity Fractures: A Systematic Review. Injury. 2018;49(2):177-183. (HUMAN)
•Diabetes Mellitus can cause a wide range of musculoskeletal disorders such as painful tendinopathies, tendon contracture, tendon rupture, and rotator cuff tear.
Ahmed AS. Does Diabetes Mellitus Affect Tendon Healing?. Adv Exp Med Biol. 2016;920:179-184. (HUMAN)
•There is significant delay in tendon strength at the end of week 2, 4 and 6 postoperatively in the diabetic rats.
Egemen O, Ozkaya O, Ozturk MB, et al. The biomechanical and histological effects of diabetes on tendon healing: experimental study in rats. J Hand Microsurg. 2012;4(2):60-64. (RATS)
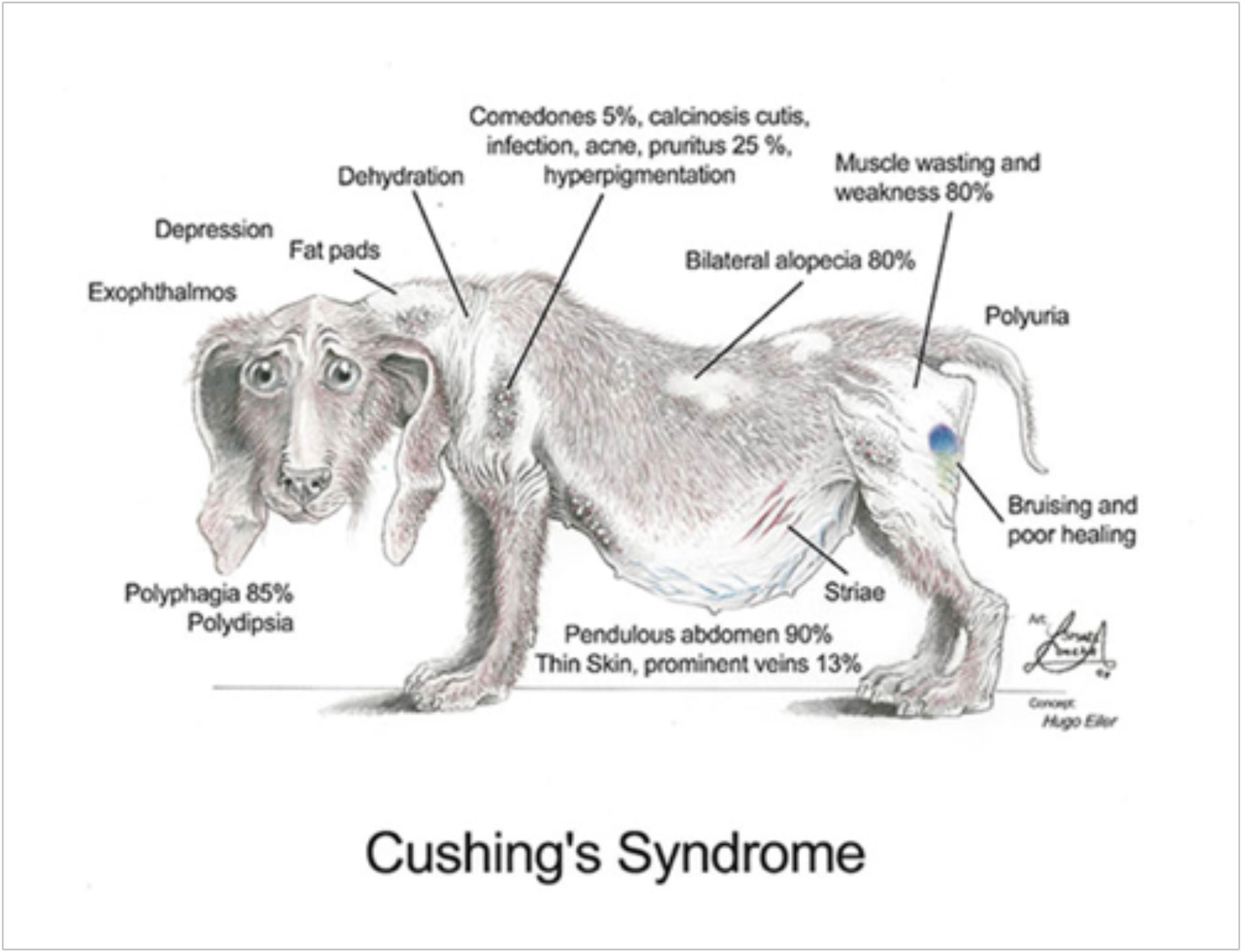
2. Cushing’s Disease / Hypercortisolism
•The classical pictures of CS includes central obesity, wasting of the limbs, proximal muscle weakness, wide purple striae, facial rounding and plethora, hirsutism with frontal balding, osteoporosis with possible vertebral fractures, hypertension and diabetes mellitus.
Galdiero M, Auriemma RS, Pivonello R, Colao A. Cushing, acromegaly, GH deficiency and tendons. Muscles Ligaments Tendons J. 2014;4(3):329-332. Published 2014 Nov 17.
•Spontanous rupture of Achilles Tendons in persons with Cushing’s Syndrome
o Mousa A, Jones S, Toft A, Perros P. Spontaneous rupture of Achilles tendon: missed presentation of Cushing's syndrome. BMJ. 1999;319(7209):560-561.
o Batisse M, Somda F, Delorme JP, Desbiez F, Thieblot P, Tauveron I. Spontaneous rupture of Achilles tendon and Cushing's disease. Case report. Ann Endocrinol (Paris). 2008;69(6):530-531.
3. Obesity
•Obese/Type2 Diabetes Mellitus tendons healed with increased expression of markers of pro-inflammatory M1 macrophages, and elevated and prolonged expression of M2 macrophages markers that are involved in Extra-Cellular Matrix deposition (subsequently increased scar tissue).
Ackerman JE, Geary MB, Orner CA, Bawany F, Loiselle AE. Obesity/Type II diabetes alters macrophage polarization resulting in a fibrotic tendon healing response. PLoS One. 2017;12(7):e0181127.
•Obesity is associated with a higher risk of tendinopathy, tendon tear and rupture, and complications after tendon surgery than non-obesity.
Macchi M, Spezia M, Elli S, Schiaffini G, Chisari E. Obesity Increases the Risk of Tendinopathy, Tendon Tear and Rupture, and Postoperative Complications: A Systematic Review of Clinical Studies [published online ahead of print, 2020 Apr 14]. Clin Orthop Relat Res. 2020;10.1097/CORR.0000000000001261.
•The High Fat-diet mouse model of obesity and Type2 Diabetes reproduces the impaired tendon healing that is observed in this patient population. The exact mechanism is unknown, but we hypothesize that a cellular defect, perhaps involving insulin resistance, leads to decreased proliferation or recruitment to the injury site, and ultimately contributes to defective tendon healing.
David MA, Jones KH, Inzana JA, Zuscik MJ, Awad HA, Mooney RA. Tendon repair is compromised in a high fat diet-induced mouse model of obesity and type 2 diabetes. PLoS One. 2014;9(3):e91234. Published 2014 Mar 21.
4. Age
•This study found that collagen fibril diameter was not altered with increasing age in the healing rabbit patellar tendon.
Sklenka AM, Levy MS, Boivin GP. Effect of age on collagen fibril diameter in rabbit patellar tendon repair. Comp Med. 2006;56(1):8-11.
•Thus, we conclude that regardless of age after maturity, tendon healing ultimately results in a substandard outcome.
Mienaltowski MJ, Dunkman AA, Buckley MR, et al. Injury response of geriatric mouse patellar tendons. J Orthop Res. 2016;34(7):1256-1263.
•We conclude that in the rabbit model MSCs do not lose their benefit as a tendon repair therapy with aging and that MSCs can be cryogenically stored for 3 years and still effectively repair soft tissue injuries.
Dressler MR, Butler DL, Boivin GP. Effects of age on the repair ability of mesenchymal stem cells in rabbit tendon. J Orthop Res. 2005;23(2):287-293.
Myopathy in patients with Diabetes, Cushing’s, Obesity, or Age
1. Diabetes
•The force deficit in db/db muscles was caused by atrophy and failure of neuromuscular signal transmission related to motor nerve axonal dysfunction. The slowed relaxation rate generally observed in diabetic muscles can, to a large extent, be explained by decreased SERCA (sarcoplasmic reticulum Calcium adenosine triphosphatase protein) pump content.
Bayley JS, Pedersen TH, Nielsen OB. Skeletal muscle dysfunction in the db/db mouse model of type 2 diabetes. Muscle Nerve. 2016;54(3):460-468.
•Sarcopenia and dynapenia have recently been recognized as a diabetic complications in type 2 diabetes. We firstly indicated that sarcopenia was frequently observed in 16.6% of patients with type 1 diabetes aged even over 40 years. Additionally, we recently reported that the prevalence rate of dynapenia was higher than sarcopenia in patients with type 2 diabetes. Chronic hyperglycemia accelerates accumulation of advanced glycation end products (AGEs), which causes diabetic vascular complications through oxidative stress and chronic inflammation.
Mori H, Kuroda A, Matsuhisa M. Clinical impact of sarcopenia and dynapenia on diabetes. Diabetol Int. 2019;10(3):183-187. Published 2019 Jun 19.
2. Cushing’s Syndrome
•CS affects muscle strength in the acute phase, but functional impairment remains detectable also during long-term follow-up despite biochemical remission.
Berr CM, Stieg MR, Deutschbein T, et al. Persistence of myopathy in Cushing's syndrome: evaluation of the German Cushing's Registry. Eur J Endocrinol. 2017;176(6):737-746.
•Similar to published data in ageing medicine, Cushing's syndrome patients show loss of muscle function that cannot be explained by loss of muscle mass. Impaired muscle quality due to fat infiltration may be the reason.
Drey M, Berr CM, Reincke M, et al. Cushing's syndrome: a model for sarcopenic obesity. Endocrine. 2017;57(3):481-485.
3. Obesity
•Obesity-linked insulin resistance is mainly due to fatty acid overload in non-adipose tissues, particularly skeletal muscle and liver, where it results in high production of reactive oxygen species and mitochondrial dysfunction.
Di Meo S, Iossa S, Venditti P. Improvement of obesity-linked skeletal muscle insulin resistance by strength and endurance training. J Endocrinol. 2017;234(3):R159-R181.
•At present, lifestyle interventions incorporating both diet-induced weight loss and regular exercise appear to be the optimal treatment for sarcopenic obesity.
Bouchonville MF, Villareal DT. Sarcopenic obesity: how do we treat it?. Curr Opin Endocrinol Diabetes Obes. 2013;20(5):412-419.
4. Aging
•Exercise training can partially reverse the age-related physiological decline and enhance work capacity in the elderly.
Mendonca GV, Pezarat-Correia P, Vaz JR, Silva L, Almeida ID, Heffernan KS. Impact of Exercise Training on Physiological Measures of Physical Fitness in the Elderly. Curr Aging Sci. 2016;9(4):240-259.
•We conclude that: (i) a multicomponent exercise training program has beneficial effects on muscle mass and physical function and should therefore be recommended to frail, obese older adults, and (ii) regular multicomponent exercise increases the basal rate of muscle protein synthesis without affecting the magnitude of the muscle protein anabolic response to feeding.
Villareal DT, Smith GI, Sinacore DR, Shah K, Mittendorfer B. Regular multicomponent exercise increases physical fitness and muscle protein anabolism in frail, obese, older adults. Obesity (Silver Spring). 2011;19(2):312-318.
So, really, all but Aging, have an impact on healing and building muscle. What does that mean for us in the rehab world?
a) We should tell the animal owner that healing will take longer and/or be incomplete
b) We need to prepare ourselves that healing with take longer and/or be incomplete
c) We may need to spend longer in each phase of healing (as judged by functional abilities or impairments versus ‘time’)
d) Maybe Medically Challenged patients need some additional time spent on targeted strengthening exercises (focusing on quads and glutes in the case of a ruptured ACL case) because a standard protocol might not yield the same recovery.
I’m sort of thinking out loud on this one! But there is no other guidance for us. Throw me your comments if you have any to share!
All the best! Cheers, Laurie