Laurie's Blogs.
Apr 2023
Stifle pain but no cruciate disease... now what? (part 2)
GUEST BLOG
Mello is a male Malinois that presented at 22 months of age with an acute onset non-weight bearing left hindlimb lameness that occurred during a fall while running. The owner immediately rushed Mello to a neighbouring hospital, where radiographs were taken and a diagnosis of partial cruciate ligament tear was made. Mello was referred to us for TPLO surgery.
When I first met Mello, he was not coping well with the 2 weeks of exercise restriction that he had endured so far. This confounded our ability to get a detailed examination. Mello is a sweet boy, but he is also very much a Mal, with all the emphatic enthusiasm that comes with being young, high drive, and restricted to 10-minute leash walks. On examination, Mello was repeatedly painful on stifle extension, intermittently reactive when attempting a drawer test, and also on palpation of the distal semimembranosus muscle.
The referring vet’s radiographs however showed a normal left stifle – no effusion to indicate intra-articular inflammation. This created a disconnect between the physical examination findings and imaging findings, enough to put the original diagnosis into question. Because the radiographs were taken so soon after the inciting event, I thought that perhaps the reason no effusion was present, was that fluid did not yet have time to accumulate. Therefore, we agreed to re-admit Mello on the next available surgery day, sedate him, and repeat the radiographs. If an effusion could be seen on repeat radiographs, we would proceed to stem cell therapy (the owner elected for that instead of a TPLO after a long discussion of the pros and cons of each). If the repeat imaging did not support a diagnosis of cruciate disease, then we would turn to other diagnostics instead.
Repeat imaging revealed a normal stifle (Figure 3), so we performed a diagnostic arthrocentesis to see if there was any evidence of intra-articular inflammation, and ultrasounded the caudal aspect of the stifle. Both the cytology and the ultrasound results came back normal.
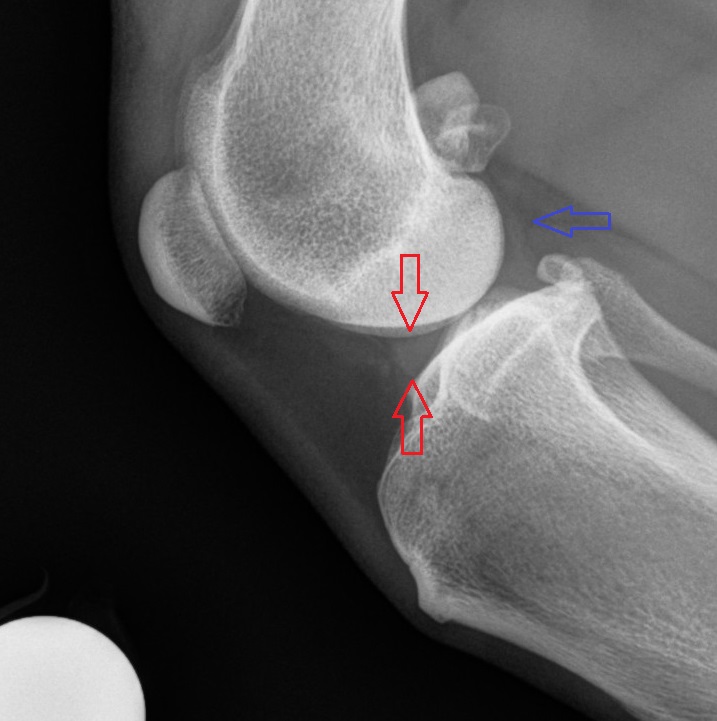
Figure 3: Normal lateral stifle radiograph. A normal amount of joint fluid can be seen, as demonstrated by a clear outline of the meniscus (between red arrows), and a lack of compression of the fat line caudal to the joint (blue arrow)
Crap. Ok then. Back to the drawing board.
To facilitate a better examination, I recommended addressing Mello’s “enthusiasm” with preveterinary pharmaceutics (gabapentin and trazadone), but the owner elected instead to provide a high value rawhide distraction chew. This worked surprisingly well; Mello focused on that thing like it had wronged him in a previous life, no longer caring whether I was fiddling around with his back leg or not. As a result, I was able to perform a much more detailed examination.
This time, I was able to localize consistent pain along the caudal medial border of the mid diaphysis of the tibia, just distal to the insertion of the gracilis, and deep to the gastrocnemius – the long hallucis flexor muscle. With Mello still focused on his toy, we returned to the ultrasound room and took some additional standing images. We then administered 2000 shocks of rESWT over the painful area, followed by 16J/cm2 of laser therapy.
The additional ultrasound images also showed no lesions. However, the owner reported substantial improvement immediately following that day’s treatment. We then prescribed and additional 2 rounds of rESWT plus laser, as well as rehabilitation therapy (performed at another facility). A month later, Mello had returned to 1 hour of off leash activity/day. The plan is to return him to full activity over the next month.
Mello’s case made me aware that I am not methodical enough in my examination of hindlimb extension injuries; that I wasn’t appropriately considering the position of the tarsus or foot while palpating stifle extension. Perhaps if I have been more meticulous, I would have picked up on the true diagnosis earlier. To that end, I reviewed the origin, insertion and action of a number of muscles that I don’t routinely see as being a cause of hind end lameness, and have modified my examination process to better isolate them.
At this stage, I’m not sure how effective these modifications will be (for instance, although I now couple external rotation with stifle extension to better test the popliteus muscle, but I’m not yet sure if that actually works or not because I don’t see a lot of popliteal injuries). Please note that any of the following stretches could yield positive results due to joint pain involving the stifle, tarsus, or pes. It’s also worth noting that truly isolating individual muscles by testing PROM alone is difficult at best, so nothing listed below should be taken as an absolute truth.
Suggested format for examining hindlimb extension injuries:
- Check for point tenderness of all relevant musculature
- Hyperflex the hip with the stifle also flexed, looking for lower lumber, SIJ, gluteal and other lumbopelvic issues. There usually needs to be substantial lower back pain (LBP) for this position to be uncomfortable.
- Flex the hip with the stifle in full or near full extension, while concurrently palpating the hamstring muscles. Reduced flexibility or pain during this stretch could reflect either a hamstring issue or LBP.
- Extend the stifle in isolation by applying caudal pressure to the patella, with the other hand holding the tibia, and with the hip in a standing angle, leaving the tarsus to extend naturally. Be aware that even at a standing angle, reluctance to extend the stifle can still be a reflection of LBP instead of an appendicular injury; repeat the test with the hip slightly extended to see if discomfort persists, and/or treat the LBP before repeating the test. Externally rotate the extended stifle to stretch the popliteus muscle.
- Repeat the stifle extension as above, but this time also concurrently flex the tarsus by applying pressure to the metatarsus (ie: tibial compression test) to include the common and gastrocnemius components of the calcaneal tendon. Repeat with the stifle in various degrees of extension to see if some positions are more comfortable than others.
- Repeat the tibial compression test as above, but this time with an emphasis on concurrently extending the digits as you extend the stifle to assess the superficial and deep digital flexor muscles. For greater precision, repeat while extending P3s only (DDF), and while flexing P3s and extending P2s (SDF).
- With the stifle flexed, flex the tarsus both in isolation, and with concurrent extension of the digits to isolate the caudal tibial, long hallucis flexor, and long digital flexor muscles/tendons.
A short “cheat sheet” version of the above can be seen in this boxed text (Figure 4)

Dr. David Lane owns and practices out of Points East West Veterinary Services in Squamish, British Columbia. You can learn more about his practice at: www.pointseastwest.com